Pregnant women with a cerclage pessary
No decision about you without you!
Medical questions to discuss with your physician
How can I find a physician with experience in pessary treatment?
Pessaries can be inserted by your physician if this is clinically indicated. For physicians unfamiliar with the Arabin pessary, instructions are provided within each package and also as a pdf-file at www.dr-arabin.de. If your physician has little experience with pessaries, you should be referred to units and obstetricians who do have such experience. Some of them are listed for different countries on our home page. There are different health care structures across the world. Some systems have specialist preterm birth prevention clinics, other systems rely on a generalist obstetrician to have a bit of knowledge of every area of pregnancy. This can lead to large variation in knowledge as it can be difficult to keep on top of all new developments in healthcare. Not every clinician will be familiar with the pessary. Therefore you should always ask for the instructions and label of the package (Figure), which indicates the size and charge number of the pessary. This can be shown to the physician in charge if you are readmitted into the hospital unexpectedly. It is important to attend hospital if you have contractions, loss of amniotic fluid, or bleeding. If you feel that your questions are not properly answered, you may write to: info@dr-arabin.de. We will try to answer within 1-2 working days.
No decision about you without you!
How can my doctor select the right size?
Your physician should read the instructions or visit the home page where we placed an automatic calculator which needs your individual characteristics. It can be found at: https://www.dr-arabin.de. Select cerclage-pessary and size. This advice is based on our own experience and will be accurate for most women. However, this is not an absolute rule, and your physician should examine you personally to ensure you receive the best fitting pessary. You should always remember that if you feel significant discomfort or pain after pessary insertion, you should report your complaints and your physician may consider a change in size.
No decision about you without you!
What is the difference between a cervical pessary with or without wholes?
The shape of perforated (ASQ) and unperforated pessaries is identical. Increased vaginal discharge is the most common side effect of the pessary. We added holes to allow the discharge to drain and to reduce the surface area of the pessary. The holes do not make a difference to the therapeutic effect of the pessary. Both designs support the cervix aiming to prevent preterm birth.
No decision about you without you!
What is the difference between a pessary which is dark blue or transparent?
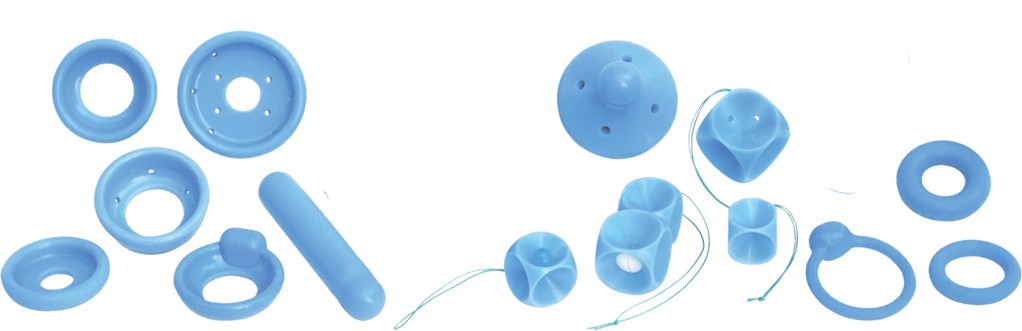
Up to 2014, the cerclage pessaries were manually produced and were blue in color (Figure left). We improved the design to use less colorant so that any impurity can be easily detected (Figure right). The new design was approved by the Food and Drug Administration (FDA) for research. The dark blue cerclage pessaries are either old or imitations where we cannot guaranty that the material has the same attitudes as tested for the transparent devices by extensive research in compressibility, cytotoxicity, sensitivity and biological tests. If unexperienced physicians may find that the color resembles amniotic membranes during speculum investigation, you may remind them that you carry this transparent blue pessary. Figure right: Transparent Arabin® pessary licensed by design, certified on a yearly basis after extensive mechanical, biological and clinical research.
No decision about you without you!
When is the cervical pessary best inserted?
The time or week of pregnancy when a pessary is best inserted depends on the following characteristics:
- Your obstetric history (risk factors for preterm birth e.g. conization, previous preterm birth, twins in the present pregnancy)
- The cervical length
- A possibly rapid change in cervical length
You should be re-assured by your obstetrician that she or he will consider all these things when making the decision to offer you a pessary. When several risk factors are present, it seems better to start earlier in gestation and/or with earlier signs of threatening preterm birth.
No decision about you without you!
How do I know that a cervical pessary is placed correctly?
After insertion of a pessary you should get up and walk without feeling any discomfort. If it is painful the pessary is not inserted correctly and your treating doctor should examine you to check the position. Your gynecologist should arrange a check-up to ensure that the pessary does not move once it has been inserted. She or he should have studied and then pass you the instructions in case you see another gynecologist unexpectedly (Figure).
No decision about you without you!
Can a pessary be used in spite of a previous miscarriage or a termination of pregnancy?
Having a previous miscarriage or a termination of pregnancy does not prevent you from having a pessary fitted if it is required. In case of repetitive late miscarriages pregnant women should be advised early in pregnancy by experienced specialists to discuss the best options of therapy.
No decision about you without you!
Can two pessaries be used (cervical & prolapse pessary)?
As far as we know, that has not yet been performed and we would not advise this due to the discomfort of wearing two pessaries and risk of necrosis of the cervix. In cases of severe genital prolapse without cervical shortening a club pessary (like a Gelhorn pessary, see Figure) better holds the organs and this may allow walking and relief of the symptoms.
No decision about you without you!
Can a pessary be used in (twin) pregnancies after IVF?
IVF itself is not a reason to need a pessary. However, patients after IVF treatment have an increased risk of preterm birth in singleton and twin pregnancies. Therefore cervical scans should be performed to monitor the pregnancy. A pessary can be used if a short cervix is detected.
No decision about you without you!
When the pessary should be removed?
The pessary should be immediately removed when you have signs of imminent delivery with painful contractions. If you are due to have caesaren section, removal must not be forgotten. If you are unsure if the healthcare team has removed your pessary, always ask. If your waters have broken your pessary should be removed as soon as possible to avoid infection. It may be kept in to allow you to transfer to another hospital if it is better for your baby to deliver in a hospital that has better facilities to look after a very small baby. Only in very exceptional circumstances should a pessary be kept in and these will be explained to you by your healthcare team.
No decision about you without you!
Lifestyle and own decision making
Can I insert or remove the pessary myself?
NO, because Arabin pessaries for preterm birth prevention are not the same as gynaecological pessaries to treat vaginal prolapse. Gynecological pessaries are increasingly inserted and removed by patients themselves. These devices are only needed when patients are exposed to increased physical stress. In the evening, these pessaries are then removed. The cervical pessary used in pregnant patients has different goals:
- It is inserted as high as possible in the vaginal fornix, to support the cervix, therefore it does not dilate the vagina.
- It is unlikely that it will be disturbing during sexual intercourse as it is positioned high at the level of the cervix, however, it may be felt.
- The device changes the utero-cervical angle in patients with a short cervix when any manipulation and prostaglandin secretion should be avoided.
Therefore, the pessary should stay in place and only be changed if clinically indicated. Some pregnant women requiring a pessary may also have a degree of womb (uterine) prolapse. Then the pessary will sit lower and may be felt more easily on examination. This is not a cause for concern; the pessary will remain positioned around the cervix.
No decision about you without you!
Can I do anything about discharge?
You should be warned by your care provider about the possibility of increased or watery vaginal discharge. This is not a reason to remove the pessary. The discharge can pool when lying down. It may appear heavier when you stand up and is allowed to drain with gravity. Many women report that it is worst getting out of bed in the morning after the discharge has collected overnight. The discharge can be heavy and it has been mistaken for the waters breaking or a vaginal infection. If you are uncertain, you should be reviewed by your local healthcare provider. But not every woman will experience discharge. Daily hygiene should be similar as in a pregnancy without pessary. No specific soap for cleaning, underwear, or treatment with lactobacillus “good bacteria” is recommended. If you have heavy discharge, you may want to wear a sanitary towel or panty liner to keep sensitive skin dry.
No decision about you without you!
When can a patient with a pessary stay at home or should be hospitalized?
Women with “only” cervical shortening, without contractions or co-morbidity are usually not hospitalized, particularly if the social conditions at home provide a supportive environment. In fact, treatment with a pessary can additionally encourage patients to stay at home instead of being hospitalized. In case of early cervical shortening or additional risk factors such as severe funneling, membrane separation, your physician should decide whether this indicates hospital admission. In patients with no inner measurable cervical length, but enough external cervical tissue to hold a pessary, indomethacin can be used for 24–48 hours before pessary insertion with a patient advised to stay in Trendelenburg position. This reduces amniotic fluid volume, alleviates pressure on the internal os and may reduce prostaglandin release before insertion of a pessary. During hospitalization, the cervical structure can be assessed. If there are no additional symptoms, the cervix remains stable and gestational age advances, the patient can later be discharged. Please attend hospital for review if you have vaginal bleeding, abnormal discharge, you think your waters may have gone, the pessary is causing you pain or you think that you may be in labour.
No decision about you without you!
Can I move (walk) with a pessary?
Yes, the pessary supports the cervix during physical activities. Most patients tell us that the pessary provides relief during physical strain such as walking or standing.
No decision about you without you!
Can I swim with a cervical pessary?
Yes, providing your cervix is closed. Ask your doctor if you are allowed to swim. Exercise in pregnancy is recommended in many countries, and swimming is considered by many to be an ideal activity for pregnant women. In women where the cervix has begun to dilate, bacteria may enter the cervix and swimming is not recommended.
No decision about you without you!
Can I have intercourse with a cervical pessary?
Sexuality is an important part of health and well-being. There is no evidence that intercourse can induce preterm birth, but there are concerns that if the cervix is stimulated it may release prostaglandins triggering labour. Depending on your individual circumstances, your doctor may advise you to avoid having sexual intercourse in pregnancy if your risk of preterm labour is very high. When a pessary is inserted around the cervix this should not affect satisfaction during intercourse. In patients with genital prolapse, the cervix will be lower and the pessary might be felt during intercourse.
No decision about you without you!
The pessary looks big. Is it painful to insert a pessary?
Vaginal health is a sensitive topic, several things can cause disruption of the balance in the vaginal flora. Women who use gynecological pessaries later in life are advised to use different cremes. But during pregnancy, when the vaginal mucosa is additionally supported by the high concentrations of estrogens, this is rarely indicated, but not contraindicated to use in case of vulvar or vaginal irritation. The physician may use lubricant to make insertion easier. Most women do not require any pain relief. However, if you find insertion very uncomfortable the physician may wish to examine you first to check for causes of discomfort (e.g. thrush) and discuss with you pain relief options that are available.
No decision about you without you!
When to ask for an extra control during treatment?
If you experience increasing discomfort, bleeding, abnormal discharge or you think your waters may have broken you should be seen by a doctor. If there are no suspicious findings, you can be re-assured, otherwise there might be an indication to reposition, to remove or change the size of the pessary. Your doctor will arrange any further routine follow up and arrange the pessary to be taken out at an appropriate time.
No decision about you without you!
Does the pessary lose its function over time?
The strength and compressibility of the silicone does not change during pessary treatment in pregnancy. The shelf life of the devices if stored under normal conditions (temperatures between zero and 40° C, without exposure to radiation) is approved to be used for a maximum of 10 years.
No decision about you without you!
In which countries is the cervical pessary available?
In Europe, the Arabin cervical pessary® is licensed by MedCert for the indication to prevent preterm birth (Identification number: MED/CERT0482 EN ISO13485 Council directive 93/42/EEC concerning medical devices). In many countries, it can be ordered by pharmacies or main distributors which are listed on the web site www.dr-arabin.de. Other requests can be made to info@dr-arabin.de. On the web site we list countries where the pessary is already registered by the national medical device institution. Registration is completed for:
- All EU countries (including GB and Israel)
- Russia
- South America (e.g. Brazil, Chile, etc.)
- Australia
- Asia (e.g. Malaysia, Thailand, Vietnam, Iran, Arabian Emirates, Dubai, etc)
- In the US and Canada, the Arabin pessary is now under investigation and it can be used within prospective studies by an FDA exemption.
- For Africa and India, we have withheld the delivery of pessaries up to now because there should be a basic health control of pregnant women to guaranty proper indication, insertion and removal.
No decision about you without you!
Health care providers of pregnant women with cerclage pessaries
Dare to care!
Preferably practical questions
Do doctors need training before treating patients with pessaries?
National boards should strive for preterm birth clinics with experienced specialist. This relates to the complex prevention of preterm birth. Although first symptoms of precocious cervical ripening may be silent, the child will be at risk for later neurodevelopmental, metabolic or cardiovascular disease. To be trained in transvaginal sonography is prerequisite to document (endo)cervical length, the utero-cervical angle or funneling. In patients with a history of anatomic malformations, cervical lesions or conization an additional speculum examination should be performed before indicating a cervical pessary. Most frequent side effects of pessaries -an increase of discharge- should be communicated. Technical training in pessary handling is useful. The clinical course may require modifications or additional treatments. It might take time to be experienced in unexpected situations because there are differences in:
- Maternal size, anatomy, parity and culture
- Pre-existing cervical shortening/thickness, opening of the internal/external cervical os
- Sensitivity to vaginal procedures (vaginismus, pain, discomfort)
- Specific obstetric situations (e.g. uterus bicornis, placenta previa etc.)
- Degree of genital prolapse or additional urinary incontinence
- Incidental or suddenly arising preterm contractions or bleeding during treatment
- Degree and kind of discharge, differential diagnosis: PPROM/ urinary incontinence
- Degree of cervical edema before removal due to contractions/pressure
It has been shown that success rates of pessary treatment increase with experience of physicians or departments by a learning curve. This also requires a basic training as demanded by the European Guideline on Prematurity. The use of medical devices is regulated by the MEDICAL DEVICE REGULATION (MDR): The manufacturer must provide instructions/ website material which is regularly modified according to post-market surveillance which must be followed. Otherwise, physicians are obliged to argue in the charts why they do not follow these instructions.
Dare to care!
What are the key points before cervical insertion?
Explain the indication, evidence, function, and side effects (discharge) of the pessary to the patient. Place the patient in a semi-recumbent position, perform a transvaginal sonography, use centile curves of the cervical length for the indication (e.g. Salomon et al.). In risk patients it is recommended to indicate a pessary earlier (cut-off 10-25th centile) than in screening patients (cut-off 5-10th centile). Chose the size according to clinical findings and instructions:
- a) the outer lower diameter should be 65mm for nulliparous or small women and 70mm for multiparous or tall women
- b) the heights of the curvature should be 17mm rarely during the first trimester, 21mm for singleton pregnancies and smaller women, 25mm for multiple pregnancy and taller women, 30mm: rarely in women with genital prolapse
- c) the inner upper diameter should be 32mm and rarely 35mm for a wide cervix or U-shaped funneling to avoid further prostaglandin secretion.
These are relative indications which can be modified for individual patients. Sizes may be changed in case of discomfort or displacement. We provide an automatic calculator for pragmatic advices on the web site: www.dr-arabin.de. A table is published in a paper: Arabin and Alfirevic, 2013, this is provided on the website as a pdf-file. Take the label of the package and stick it into the patient charts. It indicates the size and charge number. Pass the instructions to the patient and write the size and charge number on this paper in case she meets other gynecologists so that they know what was done. Fold the pessary with the smaller diameter upwards, the device should be directed towards the posterior fornix. During insertion, the pessary stays longitudinally folded until the upper vaginal fornix is reached and is then gently “pushed” as high as possible into the posterior vaginal vault with the smaller diameter around the complete cervix. The anterior rim may be gently pushed towards the sacrum. Ask the patient to get up and to indicate whether she feels comfortable. Perform only a vaginal swab if there is a high risk of PTB to inform neonatologists. Avoid inserting a pessary when contraindicated (signs of chorioamnionitis, active contractions, genital prolapse Grade III, no cervical tissue present as possibly after a previous trachelectomy). Inform the patient that in case she visits another department to provide the instructions to the physician in charge. Ask the patient for a control after one week to check the cervix and placement of the pessary.
Dare to care!
What are the key points during the course of pregnancy?
In asymptomatic patients it is sufficient to examine whether the (rotated)cervix is within the upper ring. In high-risk patients (e.g. previous PTB, short cervix at insertion, clinical symptoms) an additional TVS if possible “on top of the upper cervical part” is recommended to decide whether hospital admission and/or the application of indomethacin or corticosteroids might be indicated. Pragmatically we do not recommend to apply corticosteroids if the cervical length remains >15 mm. Bed rest has not been proven to prevent PTB, just the opposite, women doing some physical exercise have lower rates of PTB. Therefore, we allow patients with a pessary to move normally but explain her to avoid physical stress (e.g. long standing). She might feel assured to move by wearing a pessary. In case of increased discharge, the differential diagnosis with PPROM is essential to avoid ascending infection and risks of neonatal infection on one side or unnecessary removal on the other side. The differential diagnosis should imply ultrasound of amniotic fluid volume and biochemical tests. When a women carries a pessary and is admitted with preterm contractions, PPROM and chorioamnionitis should be excluded, a TVS to document the cervical structure and if contractions cannot be stopped a speculum and/or clinical examination should be performed and the pessary removed to avoid cervical lesions or increased pressure in the cervical vessels/tissue.
Dare to care!
When and how is a pessary best removed?
A cervical pessary should routinely be removed when no risk of PTB remains, at around 37 weeks. In case that a Cesarean is scheduled it might be wise to remove the device after the patient has received an epidural before skin incision if there are no contractions or PPROM. In case of proven PPROM, the pessary should be removed. There might be exceptions such as immediately before maternal transport or in case of doubtful viability when any manipulation would risk more contractions. Nevertheless, these women must be admitted and supervised by high risk specialists. To leave a pessary should be an exception after informed consent of the patient and documentation in the charts. The removal of a pessary is shown by a you tube by Prof. Alfirevic. In general, the pessary can be removed by inserting a finger between the cervix and the upper ring. It is advisable to ensure that the cervix is pushed back through the inner ring. When there are signs of cervical edema, the woman should be informed that removal may be painful. After having removed the pessary the device can be squeezed or compressed the same way as during insertion and cautiously be removed. In case the pessary is stuck due to contractions, edema or genital prolapse, it can equally be cut by scissors usually used for episiotomies instead of removing the pessary with violence. Once the pessary is removed it should not be re-used since it is certified for single use only.
Dare to care!
How to deal with excessive secretion after insertion of a pessary?
Cervical discharge is the most common side effect of pessary treatment in urogynecology but also during pregnancy. The degree of discharge depends on the individual microbiome, the material and the surface of the pessaries. It is essential to inform the patient beforehand about this side effect and to re-assure her in case she is admitted to the hospital that there is no sign of PPROM. Discharge from a pessary is not equal “chorioamnionitis or infection”. Therefore, there is no indication to treat vaginal discharge by antibiotics. New studies will evaluate whether discharge can be reduced by different materials or by the additional application of probiotics.
Dare to care!
Do we have to perform a speculum examination before/during pessary use?
There is no need to perform a speculum examination in all patients before a pessary is indicated only due to cervical shortening below a certain centile. Indications for a speculum examination before pessary insertion are:
- History of conization or trachelectomy
- History of cervical lesions
- Suspicion of uterus duplex, possibly two cervices
- Unclear interpretation of TVS
Indications for a speculum examination during pessary insertion are:
- Discomfort, suspicion of dislocation
- Vaginal bleeding
- TVS difficult to interpret
- Suspicion of PPROM – necessity to differentiate between discharge and PPROM
These are relative indications and in case TVS can answer the clinical questions it is in the responsibility of the physician in charge to decide.
Dare to care!
Is a vaginal swabs/pH detection before/during treatment indicated?
In general, the indication to perform a vaginal or cervical swab is not different from other pregnant patients with an increased risk of PTB. Meanwhile, many patients have been treated with cervical pessary and physicians should inform their patients that vaginal discharge is not necessarily combined with a change of the vaginal microbiome of each individual patient. Discharge alone should not be treated with antibiotics. Antibiotics may change the microbiome more severely. In several countries. neonatologists might wish to know the pattern of the vaginal microbiome, specifically in case of streptococcus, which should be treated when delivery is threatening. However, this also holds true for other patients at risk of SPTB. A vaginal pH measurement is performed in only a few countries to diagnose a risk of bacterial vaginosis and dysbiosis. However, the sensitivity and specificity to detect PTB has never precisely been evaluated. Nevertheless, this led to unnecessary use of antibiotics with no beneficial effect. Therefore, according to the state of the art, vaginal pH measurements cannot be advised before or during pessary treatment.
Dare to care!
How often do we perform digital/sonographic examinations?
At the first visit, it should be checked whether the upper ring surrounds the cervix, the pessary is not dislocated and still rotated towards the sacrum, all by a cautious digital examination. In care cases, the pessary might be dislocated and can be pushed upwards as high as possible with the posterior part and then rotated by slight pressure on the anterior part. A change of the utero-cervical angle and in cervical length was demonstrated by MRI. In case of additional symptoms or in patients at increased risk of PTB, an additional TVS is useful to re-assure the patient, to indicate corticosteroids or care for an admission. In case of silent progressive shortening or funneling before 30 gestational weeks the primary choice of a pharmacological treatment should be indomethacin as 100 – 200 mg/day suppositories. Any digital examination may induce prostaglandin secretion. Therefore, it might be sufficient just to feel whether the anterior rim is still rotated during follow up. Similarly, a TVS-transducer manipulation behind the cervix can be associated with prostaglandin secretion. This can be avoided by cautiously guiding the transducer “on top” of the anterior lip of the cervix until the cervical length is visualized. In case of discharge and a suspicion of PPROM or in case of vaginal bleeding of unclear origin as well as in patients with suspected dislocation a speculum examination is indicated when early removal might be indicated or prevented. In summary: A short digital examination or an anterior TVS are combined with minimal manipulation.
Dare to care!
What to do if a patient declines pessary treatment?
Every specialist should take time to explain clinical and sonographic findings and options for therapy including the most recent results. The wy of communication will have an impact whether a patient accepts or declines to accept a pessary. In very few large multiparous patients the pessary may be too small to stay in place and may dislocate. In these patients, we might adapt a customized larger pessary (produced by special modelling) or use the largest size. In patients with vaginism, it might be complicated to insert and remove the pessary due to muscular tension. Around 1/100 patients may complain to feel uncomfortable with a pessary. This can even indicate a removal of the pessary or possibly to try a smaller size, which may help that the device is tolerated.
Dare to care!
Can a physician disinfect a pessary after use?
Years ago, we evaluated whether disinfectants prevent bacterial colonization of pessaries. Since solutions and recommendations for disinfectants varies in different countries, our notified body advised NOT to recommend disinfection since not all solutions can be evaluated in terms of hygiene or changes of the material. Therefore, we do not recommend the use of disinfections before insertion any longer. The devices are tempered after production and examined by bioburden tests at regular intervals. PHYSICIANS SHOULD NOT USE THE PESSARY FOR A SECOND TIME IN ANOTHER PATIENT. If they might wish to show pessaries to their patients, physical washing might be enough to clean a pessary. Normally, the material also withstands sterilization – however, it is declared as a product for single use to avoid contamination. We provide distributors with “proof pessaries”.
Dare to care!
Preferably Theoretical Questions
Which studies are the best?
Any clinical procedures should be performed under supervision of experienced clinicians. Even the communication with patients needs experience. Although statisticians try to pretend that everything can be predicted this is not true. We live in a world of uncertainty where we also have to make fast decisions not only based on theory bit also experience. Worldwide, there are different guidelines about prevention of sPTB . The WHO underlines that screening for a disease is only recommended when the outcome can be improved. Unfortunately, after the first publication of a RCT in singleton and twin pregnancies by Goya et al. 2012 and of the sub-analysis of Liem et al. 2013 several studies were performed by unexperienced staff which might have had an impact on negative results. In several retrospective meta-analyses low-quality trials are used. The authors rarely follow the study pyramid (Figure 1). Results from these meta-analyses can be controversial when applying different selection criteria for included RCTs. Underpowered and unregistered RCTs should not be considered for any meta-analysis. It seems wise to wait for results from a running prospective meta-analysis. It cannot be expected that pessaries can prevent PTB in all patients. It has been suggested that in patients with a history of PPROM the pessary may be less effective. More studies are needed to explain the effect of pessaries in the cervico-vaginal space where the tissue is sensitive to dysbiosis. Mainly in twin pregnancies studies show benefits. Long term outcome after 3 years in children after pessary treatment demonstrate a number to treat (NTT) to prevent severe handicap or death of 1/6. In general, pessary treatment should follow the Triple Aim to increase patient satisfaction, health outcomes in a population and to reduce costs (Figure 2).
Dare to care!
Can a pessary be combined with vaginal progesterone?
Both treatments seem to be indicated in a similar group of patients with singleton pregnancies and cervical shortening. At the present stage, there are different options in case of cervical shortening to start with or even to combine both treatments. In twin pregnancies, there is no evidence that vaginal progesterone reduces sPTB (Dodd et al. 2017). Therefore, pessaries maybe preferred. This is supported by the first RCT comparing both treatments in twin pregnancies: In a predefined subgroup a cervical pessary was significantly more effective in reducing poor outcome and SPTB rates (Dang et al, 2019). One RCT randomizing patients with singleton pregnancies for vaginal progesterone, could show that the additional application of a pessary could improve the neonatal outcome by reducing PTB rates (Saccone et al. 2017). It is recommend to start any treatment earlier in pateints with additional risks as compared to screening patients. By adding vaginal progesterone to a pessary no significant impact besides a shortened stay on the NICU was found in a historic cohort (Stricker et al. 2016). More good studies are needed to compare the treatments and to select specific options.
Dare to care!
Can a pessary be combined with a cervical cerclage?
The first patient why a pessary was placed indicated by TVS was a woman who had already lost two children due to preterm birth and received a cerclage in her third (twin) pregnancy, but presented with funneling to the stich at 17 weeks. A pessary was placed on top of this cervix and pregnancy was prolonged to 37 weeks. This was an individual emergency situation. There are up to now no randomized trials (RCT) but observational case series suggesting better outcomes when a patient with a cerclage additionally received a pessary. RCTs to compare both treatment options in singleton and twin pregnancies or even combinations are still ongoing.
Dare to care!
Can pessaries be placed in women after i.m. progesterone?
Intramuscular progesterone was indicated in patients with a history of preterm birth without cervical shortening (yet) mainly in Angloamerican countries. The medication is rarely used in central Europe. The more recent PROLONG study suggests that i.m. progesterone has no beneficial effect. In Germany, 17alpha OH-progesterone Caproate (Proluton®) is not any longer available. There are no systematic studies showing that patients who already have 17alphaOH-progesterone may benefit from an additional pessary – but at least the patient can be re-assured that the pessary does no harm – since individual patients have been treated with both.
Dare to care!
What to do if the cervix is ≤ 10mm or membranes are visible?
The management should be dependent on additional clinical symptoms, the magnitude of cervical dilatation and the gestational age. Signs of chorioamnionitis and contractions should be excluded at admission. Transvaginal scans should assess the degree of funnelling, sludge, and cervical length. Before 24 weeks, obstetricians might consider cervical cerclage in singleton pregnancies. We would prefer to place or leave a pessary in place to avoid risks in case of hidden chorioamnionitis. The patient may be placed in Trendelenburg position, indomethacin (supp.) can be indicated before 32 weeks to reduce prostaglandin secretion. Dependent on the width of funnelling an upper diameter of 32mm in case of V-shaped funnelling and of 35mm in case of U-shaped funnelling should be selected. Corticosteroids or tocolytics may be indicated. A swab may be performed due to the risk of preterm birth- to inform neonatologists or to start antibiotics in case of streptococcus or resistant germs. A first still unpublished observational study in patients with funnelling showed that pessary alone is not connected with increased risks of neonatal infections.
Dare to care!
What do you do whilst waiting for the swab result?
In patients with intact membranes, we would advise to only perform a swab in case of threatening preterm birth to communicate the results to neonatologists and to exclude streptococcus. Even when swabs are performed, pessaries can be placed without delay, e.g. without waiting for the result. The use of antibiotics changes the vaginal microbiome and may result in a disbalanced pattern of benign or pathologic variants of lactobacillus. It has been proven in animals, that some bacteria can directly change the structure of the cervical tissue. Within the study of Goya et al. (2012), the type of colonization remained the same during pessary use. Within some studies a high number of patients were treated with antibiotics, which might have even increased the risk for preterm birth or cerebral palsy. Chronic infection of the decidua or membranes (increased risk after curettage or ART) does not correspond with the vaginal microbiome.
Dare to care!
How often do you add progesterone to a pessary?
In twin pregnancies: Never, see meta-analysis of Dodd et al. The meta-analysis of Romero with a positive result for vaginal progesterone was only due to one trial from Egypt which was neither placebo-controlled nor pre-registered. According to Prior these trials should not be included in meta-analyses (Prior et al.2017). A first direct comparison of pessary and vaginal progesterone showed advantages of the pessary (Dong et al. 2019).
In singleton pregnancies: Pessary treatment was our first choice in patients with cervical shortening up to 2011. After the publication of Hassan et al. we performed a historic cohort study in singleton pregnancies and added vaginal progesterone both in screening and risk patients, but did not find differences apart from a stay on NICU which might have been due to the historic model (Stricker et al. 2016 ). A first direct comparison did not show significant differences between vaginal progesterone and pessary (Cruz-Melguizo et al. 2018) in singleton pregnancies to prevent preterm birth. More studies are needed to clarify the effect of different interventions or their combined use.
Dare to care!
What if a cervix with a pessary is progressively shortening?
We do not recommend to remove a pessary to place a cerclage in patients with progressive shortening since we are afraid of amnioinfection and sepsis. It may be wise to additionally treat these patients with indomethacin supp, at least 200 mg/day before 32 weeks, to admit the patient, let her be placed in Trendelenburg and due close surveillance to exclude chorioamnionitis. It is hard to predict in which patients prolongations should be strived for. When patients have previous PPROM, several curettages or ART, chronic inflammation may be more frequently present impairing the pessary effect.
Dare to care!
Can a pessary be used in a triplet pregnancy?
Overdistension as described for twin pregnancies is even more pronounced in triplet pregnancies. Therefore, cervical shortening occurs earlier leading to higher PTB rates of triplets as compared to twins. Up to now, there are no larger trials including triplet pregnancies only. In an unpublished historic cohort in the Netherlands we could show a prolongation of pregnancies in patients with triplets, early transvaginal sonography and early pessary treatment as compared to controls without that treatment.
Dare to care!
Can cervical pessaries be used in patients with placenta previa?
Patients with placenta previa may start bleeding with cervical shortening due to a shift of layers in the lower uterine segment. Theoretically, a stabilization of the cervix may prevent cervical shortening and vaginal bleeding. The simultaneous use of pessaries with vaginal progesterone resulted in a 2.5-fold decrease in the rate of vaginal dysbiosis, bleeding and preterm birth (Barinov et al. 2016). Unfortunately, we only suspect that the effect was due to a pessary. Placenta previa is no contraindication for a pessary. Whether a pessary should be applied early in gestational even when the cervix is not shortened or whether it should be only indicated in case of precocious ripening as determined by TVS requires more research.
Dare to care!
Patients and health care providers to treat genital prolapse or stress incontinence
For patients with interest in special aspects of pelvic dysfunction we recommend our introduction video “Junction with Pelvic Dysfunction” with the link: https://youtu.be/7jrqal8Y0bM
For patients with interest in special aspects of pelvic dysfunction using a cube pessary we recommend our introduction video with the link: https://youtu.be/3ypTINfC0Yo
What is the best way to clean my pessary?
In most cases, patients can change their pessaries themselves. The frequency of change and accordingly also of cleaning may thereby vary. Cube pessaries/tandem pessaries should be removed every evening and re-inserted in the morning. The thread is attached to a fixed button in the center of the device. Cube pessaries should be cleaned every evening under running warm water, any residue can be removed with a soft toothbrush. In case of unpleasant odor, it is recommended to add a ph-neutral soap solution. For all other pessaries, the cleaning is even easier likewise under warm running water, possibly with some soap solution. Since all pessaries are only used by one patient, the devices do not need to be sterilized or “boiled”. Disinfectants are also not required, nor are they recommended, as they irritate the mucous membrane and can destroy the natural germ flora.
Can I wear my pessary during sports activities?
During horseback riding, running, jumping or dancing, complaints of prolapse or even urine loss may increase. Therefore, some women wear a pessary only during these activities, which they would otherwise not need. If a patient is already treated with a pessary, the device does not need to be removed for any sport. During swimming, all pessaries remain in place, neither chlorine nor salt water changes the silicone. While using a cube pessary without perforation, some fluid may collect behind the pessary, which can be dried off in the evening when removing the pessary. This is not associated with any risk.
Is there a risk of allergic reactions to the ingredients of the pessaries?
Allergy to silicone is extremely rare and has never been reported during the last 50 years of pessary care. All our pessaries are made of biologically compatible silicone, which is always tested by validated methods before the distribution and after a simulated period of 10 years.
What is the shelf life of pessaries?
The durability of the products as determined by “aging tests” is 10 years, which implies the function and biocompatibility during storing. From the date of the first use, our devices can be used for at least 6 months without restrictions. In case of any deficiencies detected during the first six months of use, it is advised to send us a picture with of the device and the label with the lot number. The patient will then receive a new product free of charge. Unnecessary violence such as loosening the button or “cooking” must be avoided.
How do I know which size and model is appropriate for my condition?
The variety of different pessary types and sizes are shown on our website. In general, we distinguish:
- Product family Aa: Ring-shaped pessaries for prolapse grade 1-2 and/or incontinence.
- Product family Ab: Cube/tandem or club pessaries for prolapse grade 3-4 and/or incontinence.
With regard to the size of the pessary, many physicians indicate it based on their experience. For newcomers we offer our fitting sets, which can be cleaned, sterilized, and repetitively be used. The health care provider assesses the size of a ring-shaped pessary according to the best fitting green adaption ring. For cube pessaries, there is a corresponding conversion table within the instructions.
Which pessary can be used during pregnancy to treat prolapse and/or incontinence?
The Cerclage pessary is designed to prevent preterm birth during pregnancy but can also decrease symptoms of mild genital prolapse. If the cervix is of normal length, we recommend an urethra bowl pessary for the treatment of stress incontinence during pregnancy, a sieve bowl pessary for the treatment of prolapse grade 1-2 and a club pessary for the treatment of genital prolapse grade 3-4. In addition, customized pessaries are recommended and can be requested (see first page of our website). Cube pessaries should not be used during pregnancy.
What is the reason for increased discharge?
All pessaries are a “foreign body” for the vagina; therefore, the most common side effect of pessary therapy is increased discharge.
Each patient has an individual microbiome in open body cavities such as mouth, bowel or vagina. A pessary therapy does not change the germ composition. Increased discharge does rarely indicate infections, but is most frequently the result of irritation.
We recommend the usual hygiene measures. Especially for postmenopausal women, care of the vaginal mucosa with estrogen cream twice a week, a fatty cream 7 times a week (Vaseline® or Linola®) and possibly a pH stabilization (Vagisan®). These creams can be used during insertion. If the discharge contains blood or if there is a very unpleasant odor, a physician should be consulted.
How do I use the pessary correctly?
Each pessary is accompanied by instructions on how to insert and remove the products. For the cube pessary, it is important to ensure that the thread-button combination points towards the introitus, so that the thread remains manageable. During removal the thread must not be pulled, but the vacuum effect must first be released by carefully moving it back and forth. Only thereafter, the thread can aid in removing the pessary, which is easier if one leg is leaning on a chair. If the thread is not reached, the pessary can be manually removed or otherwise a physician be consulted.
What additional treatments are indicated for urogynecological pessary therapy?
During pregnancy, no additional creams are indicated. In the pre- and postmenopausal period, pessaries should be covered with estrogen creams that help to strengthen the vaginal mucosa (e.g.: 2x/week before insertion). Daily use of a lubricating cream (e.g. Vaseline or Linola®) and a pH-stabilizing cream (e.g. Vagisan®) keep the vagina “young” and support sexual life.
Can pessaries cause pain and micturition problems?
Any pessary should improve the quality of life, not worsen it. If a pessary causes pain, problems with urination or defecation, either the type of pessary or the size needs to be modified. The gynecologist should be consulted. If in doubt, we can be contacted info@dr-arabin.de.
Should a pessary be removed during the menstruation?
Annular pessaries allow drainage of discharge and blood – there is no indication to remove these devices. After the bleeding has stopped, it is advisable to change the pessary, clean it and to remove any fibrin deposits with a soft toothbrush. Unperforated cube pessaries should not be used during the first days of bleeding. Perforated cube pessaries should be routinely cleaned every evening or more frequently, if necessary.
Is it possible to have sexual intercourse with the pessary inserted?
In general, pessaries are used for the treatment of genital prolapse symptoms and/or incontinence during daytime. Symptoms are rarely pronounced when the patient is in a recumbent position. Annular pessaries that are placed relatively high within the vagina do not interfere with sexual intercourse, nor should they be necessarily removed in the evening. Cube and tandem pessaries are removed in the evening anyway – this can be done before eventual intercourse. The coating with estrogen cream, Vaseline or Vagisan® in the morning even improves sexual life in the long term. However, club pessaries, which are only indicated for severe prolapse, may be disturbing due to the stalk.
Can I use any pessary with mechanical contraceptives?
When using intrauterine pessaries (Mirena®/Jaydess® / IUD), care must be taken not to dislodge the fine thread. When using cube pessaries, where the patient wears a pessary only during the day and removes it in the evening, special care must be taken to remove the vacuum effect. The hormone-containing vaginal rings can be left in place above any pessary. Nothing is known about the combined treatment with a diaphragm, we do not recommend it due to concern that the position of the diaphragm might be dislocated.
Can I use the pessary before and after surgery on the genital tract?
In many countries, it is recommended not to perform surgery of the pelvic floor without a preceding therapy with pessaries. International studies have shown no significant differences in terms of satisfaction and efficiency when comparing pelvic floor operations and vaginal pessaries. Another indication for pre-operative treatment is the additional application of estrogens applied on a pessary, which improves local blood supply and thus the success of surgery. Experienced specialists still indicate pessaries after surgery of the pelvic floor to stabilize the surgical result and prevent premature recurrence. This should be discussed prior to surgery.
What is a customized pessary?
A request for customized (individually made) pessaries can be downloaded at
www.dr-arabin.de (first page). The MDR (Medical Device Regulation) requires a physician’s order for the fabrication of a customized device. Health insurances should be asked whether the costs for fabrication are covered. Various models that are not commercially available can be asked for. Frequently, the forms will be individualized or metal inlays inserted (like in Hodge pessaries). New designs for the use during pregnancy and the postpartum period are developed.
Can the use of pessaries lead to a worsening of genital prolapse or incontinence?
Pessary therapy should improve the quality of life of women of all ages. In the past, it was common to leave pessaries in place for a long period. With ring-shaped pessaries, there may then be a risk of further dilatation of the vaginal walls, resulting in the need to use pessaries with increasingly larger diameters. This risk can be prevented by removing pessaries in the evening and re-inserting them in the morning. In the case of pessaries that adhere due to a vacuum effect (e.g. cube pessaries), there is no risk of additional dilatation. In fact, it is often the case that patients require smaller sizes as the pelvic tissue is massaged and strengthened by this mechanism.